Rapid and mass digitization has always been considered a band-aid solution to an inefficient public system in the world, a trend to which the healthcare industry is no exception. Focusing locally, there exist several challenges in the Indian healthcare system, as it functions in an inaccessible, fragmented, and inefficient structure. The need to dispense healthcare services to 1.4 billion citizens and overcome the digital divide called for an affordable, accessible, and consolidated health infrastructure to be created. In order to counter this problem, previous governments have made several attempts at digitizing the healthcare system and unifying data across multiple stakeholders, starting with the National Health Portal in 2014 [1]. However, these efforts have not succeeded. Presently, health data exists with over 50 lakh healthcare professionals and over 12 lakh healthcare facilities, all in different standards and formats on different platforms completely. [2] This makes the seamless exchange of health data between different healthcare providers, hospitals, and systems a herculean task. Such impediments hinder effective data-sharing practices with multiple patient profiles existing on different and fragmented databases.
To overcome all these issues, the government introduced the pilot run of the Ayushman Bharat Digital Mission (ABDM) on August 15th, 2020, in the midst of the COVID-19 pandemic. [3] Presented as the incumbent government’s flagship large-scale health digitization project, the ABDM consisted of three components: Health ID, Healthcare Professionals Registry, and Healthcare Facilities Registry. For the purposes of this article, we will be assessing the Health ID, later rebranded as the Unique Health Identifier (UHID) and then eventually Ayushman Bharat Health Accounts (ABHA). But to understand the components, purposes, and utility of a Health ID, it’s pertinent to uncover the digital foundation laid by the ABDM.
The Infrastructure Surrounding the ABDM
Under the National Health Policy of the Government of India, the Ministry of Health and Family Welfare had conceptualized the Ayushman Bharat Digital Mission, to consolidate the entire healthcare ecosystem. This was achieved by making it digitized, interoperable, and more accessible. Such a transformative initiative was aimed at revolutionizing the healthcare sector by leveraging digital technologies to enhance access to quality, reliable and affordable healthcare. It is developed on a federated architecture, which allows interoperability and portability of the personal health records of patients between independent and decentralized information systems. During the development of this system, the security and privacy of patients’ personal data were prioritized. [4]
The entire ecosystem consists of various stakeholders divided into 6 categories:
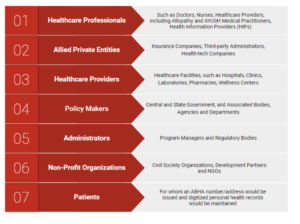
In order to provide a swift and efficient digital healthcare delivery ecosystem, the National Health Authority has integrated over 100 programmes and health applications/Personal Health Record (PHR) applications with the ABDM. [5] This includes Central programs and campaigns, such as Aarogya Setu, eHMIS, eSushrut, ESIC-Employees’ State Insurance Scheme, etc. as well as State efforts such as Haryana e-Upchaar, ANM Andhra Pradesh Health EHR, West Bengal Integrated HMIS, etc. Through this, the ABDM acts as a platform and a catalyst to unify and consolidate data from public and private healthcare initiatives, programmes and facilities. Its utility comes into the picture as all this data collected across the digital health ecosystem can be accessed easily by each patient by signing in with their ABHA number.
It achieves this through the multiple Application Programming Interfaces (APIs) with which the infrastructure is equipped, which is integrated with the existing software at hospitals and labs. This includes compiling Electronic Medical Records (EMR), Hospital Information Management Systems (HIMS), Laboratory Information Management Systems (LIMS), Telemedicine data, etc. In addition to the APIs, the government’s ABDM Sandbox environment also acts as an arena for Health Information Providers (HIPs) and Health Information Users (HIUs) to register themselves and validate their software systems using the ABDM APIs. The use of such open technology allows more and more health applications to join the ecosystem. Its success is witnessed through widespread adoption, where 919 independent health tech innovators have already registered onto the ABDM Sandbox both from the public and private sector. [6]
Members of a Federated Health Records (FHR) System
An FHR system consists of three components: HIPs, HIUs and HIE-CMs.
A Health Information Provider (HIPs) is any entity that generates or leads to the generation of health data of any patient, e.g. hospitals, health care centers, clinics, pharmacies, any form of laboratory, pathology centers, etc. Once HIPs integrate themselves into the FHR system, they automatically agree to allow the flow of health data into a patient’s ABHA account, which is accessible by any third-party only by the consent of the patient.
Once this data has been set off into the FHR system, any entity which wants access to it are Health Information Users (HIUs). The purpose of this access is to provide directed, targeted, and accurate services to the patients to whom the data pertains, e.g. hospitals, clinics, health-tech companies, health-analytics companies, insurance companies, medical researchers, government entities, etc.
For both HIPs and HIUs, access to the health data through an ABHA account can only be granted on the consent of the account holder, i.e. patient, for a limited period of time and for limited purposes. Integrating HIPs and HIUs as a part of the ABDM ensures that only verified registries exist in the digital ecosystem, that are in compliance with the mission’s health data management policy and guidelines.
Another pivotal component in the healthcare infrastructure in India are the Health Information Exchange – Consent Managers (HIE-CMs). Since health data under the ABDM is stored in a decentralized and federated manner, free from unregulated access and control by the State, the HIE-CM secures the access to and sharing of sensitive health information amongst the stakeholders. It must be noted here that neither the State nor any of its agencies store the data existing in the ABDM ecosystem, but they merely provide a gateway for its access, use and transfer. That gateway is the HIE-CM. It grants the agency and control over their health data to the patients as they are authorized to grant access, exchange and processing of their health data. In addition to this, they can restrict control and manage consent preferences, all through their ABHA accounts. Through this, patients can not only specify which healthcare providers they are comfortable sharing their data with but also can choose the duration, extent and conditions of their consent, providing them with the flexibility to tailor their data-sharing preferences. It’s the functioning of the HIE-CM that ensures a privacy and patient-centric healthcare system.
In the next part of this two-post series, we’ll explain how all of the above has been operationalized by the introduction of Ayushman Bharat Health Accounts (ABHA). We’ll further cover its benefits and the accessibility it grants, how you can be a part of this ecosystem, and how its interoperability is put into practice across different platforms, public/private healthcare services, programs, etc.
Footnotes
[1] MoHFW Launches National Health Portal, PIB Press Release, Ministry of Health and Family Welfare (Dec. 16th, 2014), https://pib.gov.in/newsite/PrintRelease.aspx?relid=113443.
[2] A Brief Guide on Ayushman Bharat Digital Mission and its Various Building Blocks, National Health Authority (2022), https://abdm.gov.in:8081/uploads/ABDM_Handbook_19_10_2022_24c5078481.pdf.
[3] More than 15 Crore National Digital Health IDs Created under Ayushman Bharat Digital Mission, PIB Press Release, Ministry of Health and Family Welfare (Feb. 4th 2022), https://pib.gov.in/PressReleasePage.aspx?PRID=1795425.
[4] Ayushman Bharat Digital Health Mission: Draft Health Data Management Policy, National Health Authority (Apr. 2022), https://abdm.gov.in:8081/uploads/Draft_HDM_Policy_April2022_e38c82eee5.pdf.
[5] Over 100 Programmes, Applications Integrated with Ayushman Bharat Digital Mission, ANI (May 11th, 2023), https://www.aninews.in/news/national/general-news/over-100-programmes-applications-integrated-with-ayushman-bharat-digital-mission20230511204941/.
[6] More Than 50 Digital Health Services/Applications Integrated with Ayushman Bharat Digital Mission (ABDM), PIB Press Release, Ministry of Health and Family Welfare (Jul. 28th, 2022), https://pib.gov.in/PressReleasePage.aspx?PRID=1845845.
[7] Ayushman Bharat Digital Mission: ABDM PHR Fundamentals, National Health Authority, https://phr.abdm.gov.in/.